Onychomycosis: Reclaim Your Healthy Nails From Fungal Foes
Onychomycosis, often referred to as toenail fungus, is a prevalent fungal infection that affects the fingernails and toenails. This condition, while not life-threatening, can be aesthetically displeasing and sometimes cause discomfort. Fungi thrive in warm, moist environments, making toenails particularly susceptible due to the enclosed space within shoes.
This article delves into the world of onychomycosis, exploring its symptoms, causes, diagnosis methods, and various treatment options available. By understanding the signs and available solutions, you can effectively address this fungal foe and reclaim healthy, beautiful nails.

Symptoms of Onychomycosis
The signs of onychomycosis can vary depending on the type and severity of the infection. However, some common symptoms include:
- Discoloration: The nail may become white, yellow, brown, or even black.
- Thickening: The affected nail might thicken and become crumbly.
- Brittleness: The nail may become brittle and prone to breaking.
- Distortion: The nail’s shape can become distorted and irregular.
- Separation: In severe cases, the nail may separate from the nail bed (the skin beneath the nail).
- Debris: Build-up of debris under the nail can occur.
- Unpleasant odor: A mild, foul odor may sometimes emanate from the affected nail.
It’s important to note that not all changes in nail appearance indicate onychomycosis. Other conditions like psoriasis, injury, or certain medications can also cause nail changes. If you suspect onychomycosis, consulting a dermatologist for diagnosis is crucial.
Causes of Onychomycosis
Several types of fungi can cause onychomycosis. The most common culprits are dermatophytes, a group of fungi that thrive on keratin, the protein that makes up hair and nails. Yeast and molds can also be responsible for some cases of onychomycosis.
Here are some factors that can increase your risk of developing onychomycosis:
- Age: As we age, our nails become thinner and more susceptible to fungal infection.
- Medical conditions: Certain medical conditions like diabetes, peripheral arterial disease, and a weakened immune system can increase the risk.
- Wet environments: Spending a lot of time in damp environments like public pools or showers can increase your risk of fungal exposure.
- Foot injuries: Injuries to the nail bed can create an entry point for fungal spores.
- Poor circulation: Reduced blood flow to the feet can make it harder for the body to fight off fungal infections.
- Wearing tight-fitting shoes: Shoes that crowd the toes create a warm, moist environment ideal for fungal growth.
- Sharing personal items: Sharing shoes, towels, or nail clippers with someone who has onychomycosis can increase your risk of contracting the infection.
Diagnosis of Onychomycosis
Diagnosing onychomycosis involves a combination of methods by a dermatologist. Here’s what you might expect:
- Physical examination: The dermatologist will visually examine your nails, assessing discoloration, thickening, and other changes.
- KOH examination: A scraping of the nail or debris underneath it is collected and examined under a microscope with potassium hydroxide (KOH) solution. This helps identify the presence of fungal elements.
- Fungal culture: In some cases, a sample may be sent to a lab for culture to identify the specific type of fungus responsible for the infection.
These diagnostic methods allow the dermatologist to confirm the presence of onychomycosis and determine the most appropriate treatment course.
Treatment Options for Onychomycosis
Several treatment options are available for onychomycosis, and the best choice will depend on the severity of the infection, the type of fungus involved, and your overall health. Here’s a breakdown of the common treatment methods:
Oral Antifungal Medication:
- This is often the preferred treatment for moderate to severe onychomycosis, particularly when multiple nails are affected.
Medications like terbinafine, itraconazole, and fluconazole are commonly used. - These medications work by targeting the fungus systemically, meaning they are absorbed into the bloodstream and reach the infected nail bed.
- Oral antifungal medications typically require treatment for several weeks or months, depending on the severity of the infection and the specific medication used.
- It’s important to note that these medications can have side effects, and some may interact with other medications you are taking. Therefore, discussing your complete medical history with your dermatologist is crucial before starting treatment.
Topical Antifungal Medication
Topical antifungal medications are applied directly to the affected nail and are typically used for mild cases of onychomycosis or when oral medications are not suitable due to potential side effects or drug interactions. Here’s a closer look at topical antifungals:
- Types: Common topical medications include clotrimazole, miconazole, and ciclopirox.
- Application: These medications come in various forms like creams, lotions, or lacquers. The specific application method and frequency will depend on the medication prescribed. Generally, topical antifungals need to be applied regularly for several months to see results.
- Efficacy: Topical medications may not be as effective as oral medications, especially for severe infections. However, they offer the advantage of minimal side effects.
- Considerations: Consistent application is crucial for the success of topical treatment. Additionally, topical medications may not penetrate the nail plate effectively, especially in cases of thickened nails. In such situations, debridement (removal of some of the infected nail plate) may be necessary to improve medication penetration.
Laser Treatment:
- Laser treatment is a relatively new option for onychomycosis. It involves using a high-intensity laser beam to target and destroy the fungus within the nail plate.
- This treatment option is generally considered safe and effective. However, it may be more expensive than other treatment methods and might require multiple sessions.
- Laser treatment is still under investigation for long-term efficacy, and insurance coverage may vary.
Nail Debridement:
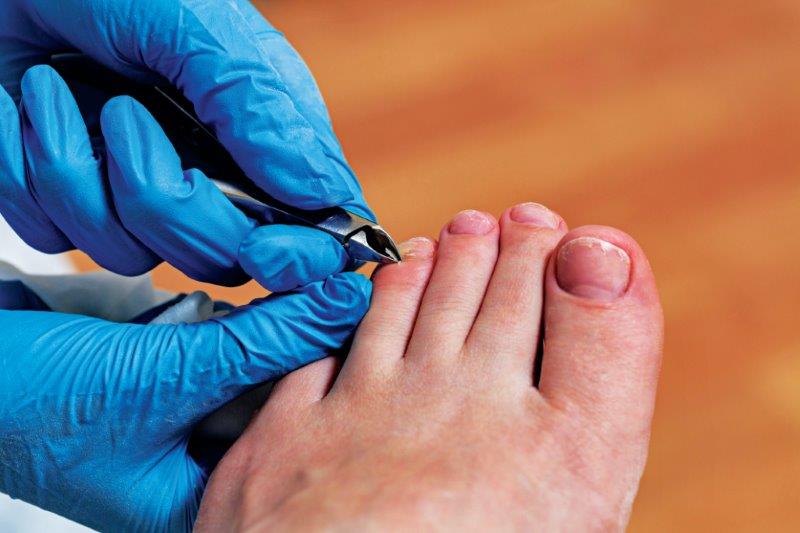
- Nail debridement involves physically removing part or all of the infected nail plate. This can be done by a podiatrist or dermatologist using various methods like clippers, drills, or lasers.
- Debridement can be helpful in conjunction with other treatment options, particularly topical medications, by allowing for better penetration of the medication to the nail bed.
- This procedure can be uncomfortable, and repeated debridement may be necessary during the treatment course.
Home Care Practices:
In addition to the above treatment methods, incorporating some simple home care practices can help manage onychomycosis and prevent recurrence:
- Maintain good foot hygiene: Wash your feet daily with warm, soapy water and dry them thoroughly, especially between the toes.
- Wear clean, dry socks: Opt for breathable cotton socks and change them daily.
- Choose proper footwear: Select well-ventilated shoes that fit comfortably and avoid tight-fitting shoes.
- Avoid sharing personal items: Don’t share shoes, towels, or nail clippers with others.
- Keep your nails trimmed: Regularly trim your nails straight across to minimize the area for fungal growth.
